You are about to leave OurWayForward.com.
You are about to leave a GSK website. By clicking this link, you will be taken to a website that is independent from GSK. The site you are linking to is not controlled or endorsed by GSK and GSK is not responsible for its content.
Understanding How Family History & Biomarkers Play a Role in Endometrial Cancer
Is Endometrial Cancer a Genetic Disease?
Endometrial cancer can have a genetic component. A family history of endometrial cancer may be associated with an increased risk of developing the disease. Read on to learn how your family history plays a role, what to ask your healthcare team about, and how to get tested.
Family History
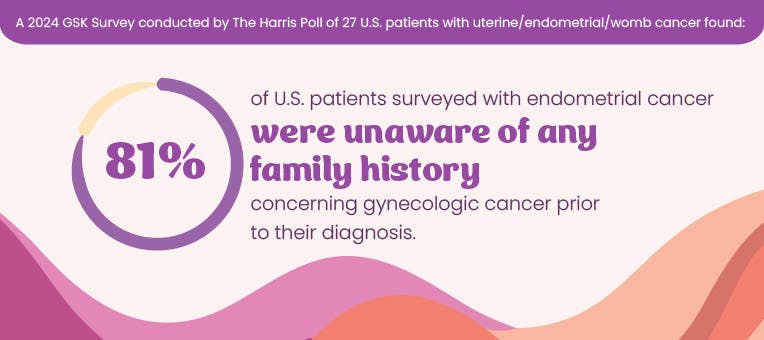
Your genes can determine many characteristics about you, such as the color of your hair, how tall you are, and whether you may be at increased risk of developing certain diseases, such as endometrial cancer. Families with a history of Lynch syndrome, a genetic condition inherited from a parent, have a higher risk of developing endometrial cancer.
How do I learn more about my family history?
To understand your own health risks, it’s helpful to talk to your family members. Here are some key pieces of information to gather:
- Their sex, date of birth, and ethnicity
- Any medical conditions they know of, and the age they were diagnosed
- Any complications they had during pregnancy or other reproductive issues
- Their lifestyle habits, such as diet, exercise, and tobacco use
It’s also important to understand the health history of any immediate relatives who have passed away.
Other places you can look for information are:
- Public records (birth certificates, death certificates)
- Obituaries
- Baby books
Having these conversations can be challenging. If you’re unsure about discussing health history with your family, consider these tips:
- Don’t go at this alone – ask a sibling or close family member to join you
- Explain why you want to gather this information
- Respect your relatives’ privacy
- Listen without judgment
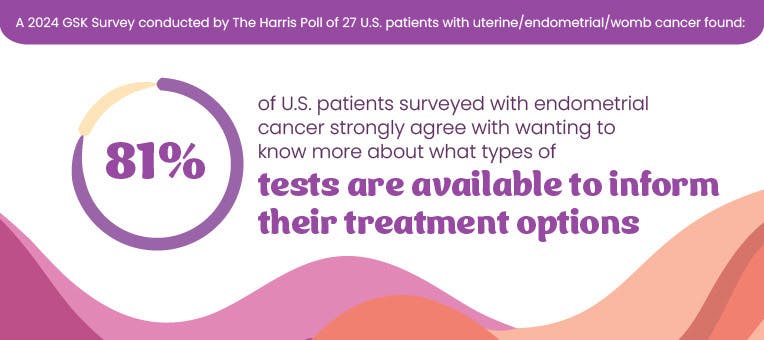
In addition to talking with family, healthcare professionals can perform molecular testing and look for biomarkers that can help determine cancer risk, prognosis, and potential treatment options.
Endometrial Cancer Biomarkers
What is a biomarker?
Biomarkers are specific characteristics found in cells, such as proteins or DNA, which can help assess your cancer risks (both of developing or disease prognosis) and treatment options. Like many other cancers, endometrial cancer has biomarkers that can be identified through testing. Key endometrial cancer biomarkers include Mismatch Repair (MMR) and Microsatellite Instability (MSI).
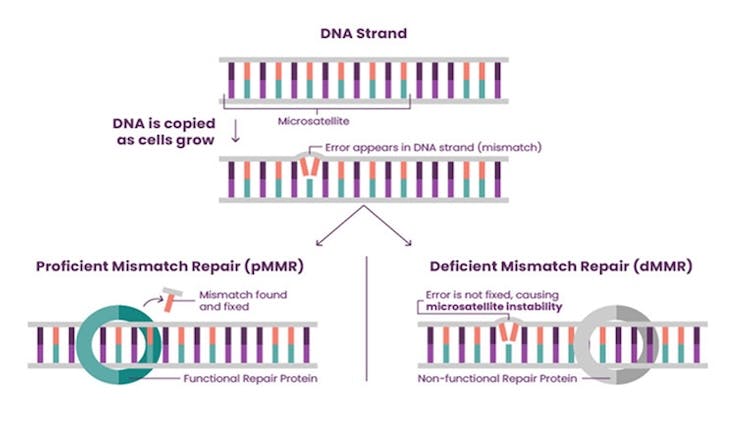
MMR and MSI in Endometrial Cancer
- In normal cells, mismatch repair (MMR) is a process that fixes errors in the short, repeating pieces of DNA, called microsatellites, when DNA is copied in a cell. This process helps keeps the genes in a cell stable.
- When this process is working correctly, it is referred to as proficient mismatch repair (pMMR). Approximately 70% of endometrial cancer tumors are pMMR or microsatellite stable (MSS).
- When this repair system does not work correctly, the tumor has deficient mismatch repair (dMMR).
- Eventually, the errors left behind do not get fixed and cause more errors within the microsatellites. This is known as microsatellite instability (MSI), which is common in cancer cells.
- Tumors that have high levels of MSI are known as MSI-High.
- Tumors that are dMMR or MSI-H are more common in endometrial cancer than other cancer types and are found in about 30% of patients with endometrial cancer.
- Understanding the MMR or MSI status of your tumor may help your healthcare team learn more about the cancer and determine appropriate treatment options. Tumors with dMMR/MSI-H biomarkers are more likely to respond to immunotherapy.
Determining MMR/MSI Status Through Testing

Immunohistochemistry (IHC)
- IHC is a testing method to determine MMR status. A piece, or sample, of the cancer tissue is taken out during a biopsy or surgery.
- IHC is completed in a lab that tests by adding a dye to the tissue sample.
- Once the dye is added to the sample, the lab technician takes a closer look through a microscope to determine biomarker status.

Polymerase Chain Reaction (PCR)
- Like IHC, PCR is completed in a lab to measure MSI by quickly making millions to billions of copies of a piece of DNA, so that it can be studied more closely.

Next-Generation Sequencing (NGS)
- NGS testing is also done in a lab, looking at DNA and RNA fragments like they are building blocks. This kind of test puts together the fragments to identify any changes in certain areas as they are placed together.
- Healthcare professionals can then choose medications that target these genetic changes in the tumor.
MMR and MSI are important endometrial cancer biomarkers, but there are other ones you may have. Below are other biomarkers associated with endometrial cancer:
- Estrogen and progesterone receptors (ER/PR)
ER/PR are hormone receptors found in about 57% of endometrial tumors. They may help predict how well a patient might respond to hormone therapy.
- Tumor mutational burden (TMB)
TMB measures the number of mutations within a tumor. About 15% of endometrial cancers have high TMB, which may be associated with both a better prognosis and better responses to immunotherapy.
- Polymerase epsilon (POLE) mutations
POLE mutations occur in about 10% of all endometrial cancers. These patients may be less likely to experience the cancer returning, tend to survive longer and appear to benefit less from chemotherapy and radiation.
- Human epidermal growth factor receptor 2 (HER2) proteins
Certain types of endometrial cancer have high levels of HER2 and are more likely to respond to therapies that target this biomarker. Lower HER2 levels have been associated with better survival rates.
- Phosphatase and tensin homolog (PTEN) gene mutations
PTEN mutations occur in about 45% of endometrial cancers. PTEN loss can serve as a warning sign that precancerous tissue is at higher risk of developing into endometrial cancer.
- Neurotrophic tyrosine receptor kinase (NTRK)
NTRK is a less common biomarker in endometrial tumors, but it can be useful for making treatment decisions. For patients who test positive for NTRK gene fusion, tyrosine kinase inhibitors (TKI) can be used to target cancer cells.
- P53 gene mutations
P53 mutations occur in about 15-25% of all patients with endometrial cancer but are responsible for 50-70% of endometrial cancer deaths. While these patients tend to have poor prognosis, they are also more likely to benefit from combined chemotherapy and radiation.