You are about to leave OurWayForward.com.
You are about to leave a GSK website. By clicking this link, you will be taken to a website that is independent from GSK. The site you are linking to is not controlled or endorsed by GSK and GSK is not responsible for its content.
Let’s Talk About Gynecologic Cancers
If you feel awkward, uncomfortable or avoidant talking about your gynecologic cancer, know that you are not alone. This page was created to help address some of the topics you may be thinking about but may not feel comfortable voicing. No matter where you are in your experience—whether you are newly diagnosed, have been living with a gynecologic cancer for a while, or are here on behalf of a loved one—the more you know, the more you can do to find your way forward.
After reading through this page, visit the Advocacy Organizations page, to find more support and resources related to the topics on this page.
Sharing Your Gynecologic Cancer Diagnosis
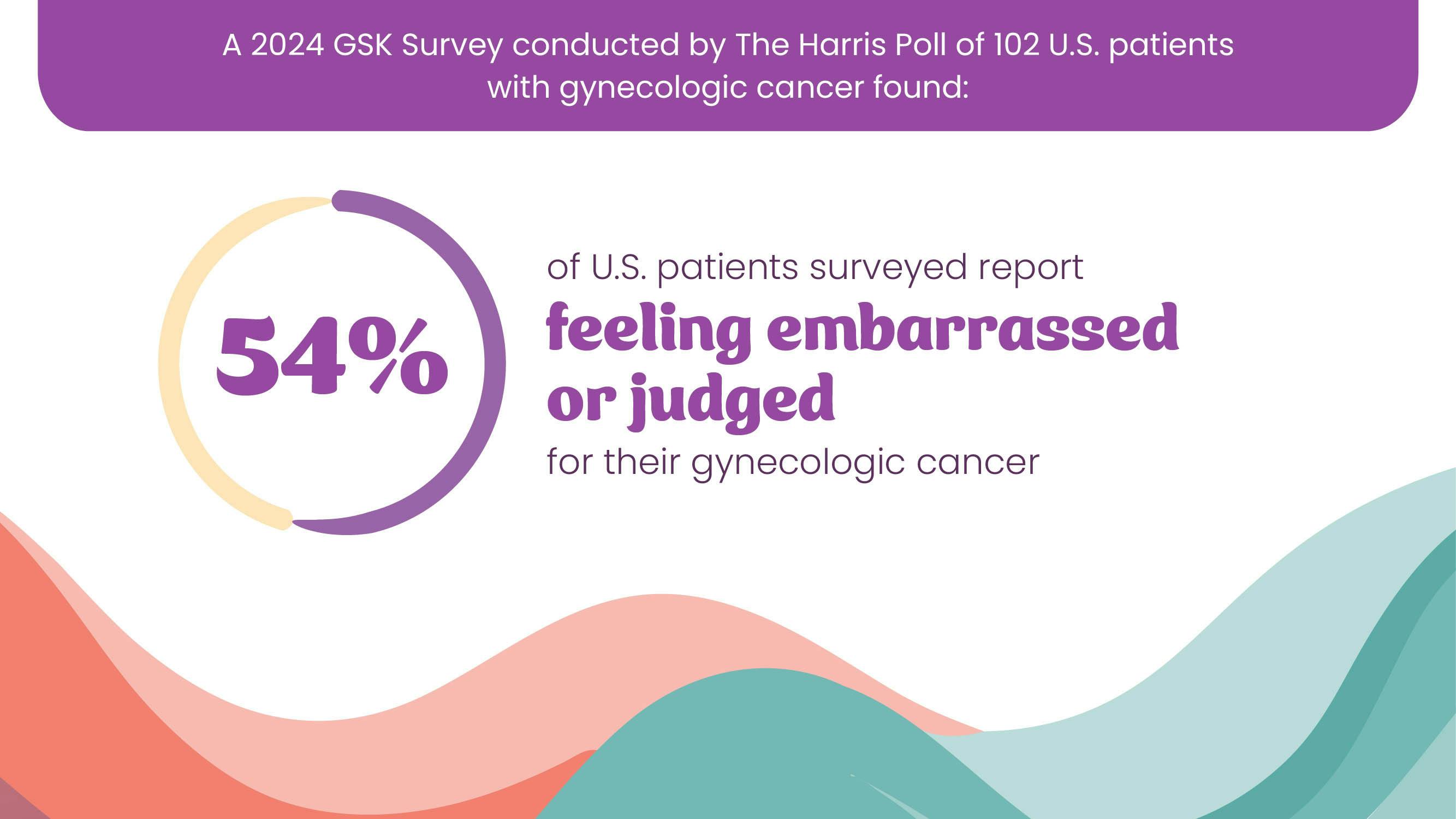
Facing any type of cancer is difficult, but facing a gynecologic cancer can bring on other, unique challenges. This can lead to feelings of isolation and may prevent you from getting the support you need. It's important to speak openly about your experiences so you can feel more comfortable and understood.
I’m worried about being judged for having a gynecologic cancer because of my culture/religion. What should I do?
- It's common to feel this way, especially in cultures where discussing your emotions and health-related care is not common.
- Seeking support from people who understand may be helpful.
- Many organizations offer support groups where others in the gynecologic cancer community share their experiences, which can help you realize that you're not alone. These groups may be able to introduce you to others with similar backgrounds to yours.
- Finding a healthcare professional who is sensitive to your culture or religion may also help you navigate these feelings.
How do I deal with feelings of shame or embarrassment?
- It's normal for some people to have these feelings and important to acknowledge and respect how you feel.
- Learning more about your diagnosis and treatment can help you better understand and discuss it.
- Talking to others who have had similar experiences can help you realize you are not alone.
- Additionally, speaking with a therapist or someone you trust can help you understand and manage your emotions.
- Recognize your strengths and the courage it takes to face your diagnosis. Remind yourself that having gynecologic cancer is not your fault.
- Remember to treat yourself with the same kindness and understanding that you would show a friend in a similar situation.
How do I cope with feeling like I’m losing a part of my identity?
- It’s common to feel this way after a diagnosis of gynecologic cancer.
- Certain cultures may connect identity with having certain body parts and how they work. Facing a gynecologic cancer can challenge those beliefs for some people.
- To help work through these feelings, consider joining gynecologic cancer support group or talking to a therapist or close friend.
Where can I go for support?
- Ask your healthcare team about local support groups and therapists who specialize in helping people with cancer.
- Advocacy organizations provide many ways to find social and emotional support.
- Social media can also be a helpful way to connect with others who are going through similar experiences.
- You can connect with others in the gynecologic cancer community by visiting the Our Way Forward social channels on Facebook, Instagram, and YouTube.
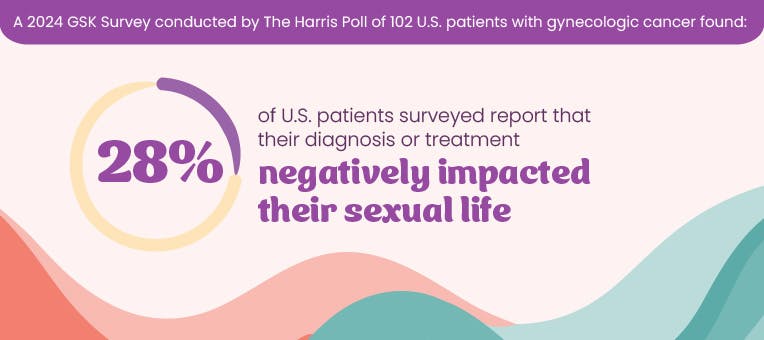
Sexual Health and Intimacy
Gynecologic cancer may affect your sex life. Treatment side effects may make your body feel different, and you may start to feel differently about sex. Additionally, you may feel uncomfortable discussing sexual health because of your identity, cultural, or religious barriers. However, sexual health is an important part of your overall well-being, and your care team can help you find the support you need.
How can gynecologic cancer affect my sex life?
- During your experience with gynecologic cancer, you may find that you have less sexual desire.
- The side effects of gynecologic cancer treatment may also impact how you feel about sex and how it feels physically. You may feel tired, or you may have vaginal changes.
- Physical changes like hair loss and changes in weight may make you feel disconnected from your body and uninterested in sex.
- It’s important to talk to your trusted health care professionals about any concerns related to your sexual health and intimacy.
How do I talk about a lack of sexual desire with my partner?
- If comfortable doing so, consider trying an open and candid approach with your partner. See if you can work together to address the challenges. You might also find it helpful to speak with a sexual health counselor, who may be available at your cancer care facility, to assist with these discussions.
Is there anything I can do to improve this aspect of my experience?
- Adapting to the changes in your body after a gynecologic cancer diagnosis can take time and practice, just like learning a new skill.
- Consider talking to your partner, trying new activities and finding ways to connect beyond sexual activity.
- Your healthcare professional may also have recommendations.
How can I navigate conversations about sexual health with my health care team, especially if it feels uncomfortable?
- It’s completely valid to feel unsure or uncomfortable about discussing sexual health, especially if your doctor might not be familiar with the unique needs of your community.
- Seek out affirming healthcare professionals who have experience addressing sexual health. Many cancer centers have specialists or offer referrals to healthcare professionals in your community who can help you navigate this more comfortably.
- If you feel comfortable, sharing personal aspects of your identity, such as gender identity, sexual orientation, or cultural considerations, may help your healthcare professional better understand your experiences and potentially provide more tailored care.
- Medical terms and recommendations can sometimes feel out of place if they don’t align with your experiences. Don’t hesitate to ask your doctor to clarify why certain aspects of sexual health are important post-treatment, even if it doesn’t seem to apply to you. For example, ask about how cancer treatment might impact your body, libido, or other aspects of your sexual function regardless of your sexual practices.
- If you feel uneasy having these conversations alone, bring a supportive friend, partner, or health advocate to the appointment. They can help facilitate the conversation and ensure your needs are heard. Advocacy organizations may be able to help you navigate this.
Fertility and Gynecologic Cancer
Gynecologic cancer may affect your fertility if you are in your childbearing years. For some, the potential loss of fertility could be more upsetting than the cancer itself.
Will gynecologic cancer affect my fertility?
- Gynecologic cancer and its treatments may affect the reproductive system. This may make it hard to get pregnant or carry a pregnancy to term.
- Whether and how your gynecologic cancer impacts fertility depends on several factors, including the type of treatment, the type of cancer, how advanced it is, age and other factors.
- It's important to discuss your fertility concerns with your doctor when you discuss your treatment plan.
- You can also ask your doctor about potential ways to preserve your fertility through reproductive technologies, like egg freezing, before you start treatment.
- Your doctor may refer you to a fertility specialist to explore your options further.
What if I get pregnant during my cancer treatment?
- In some cases, cancer treatment may not affect fertility. However, there could be concerns about the risk of birth defects if a pregnancy occurs during or shortly after treatment.
- If you are able to become pregnant, talk to your doctor about the risk of getting pregnant.
- Even if you think you can't get pregnant, but are sexually active, you should still talk to your doctor. It's important to know what kind of birth control is the safest and most effective for you to use.
- If you want to get pregnant after treatment, talk with your doctor about how long you should wait to start trying. Your doctor may refer you to a fertility specialist to discuss your options further.
Menopause and Gynecologic Cancer
Menopause is a point in time that marks the end of a person's reproductive years, defined by experiencing 12 straight months without a menstrual period. It commonly occurs between the ages of 45 to 55, due to hormonal changes. The transition includes three stages: perimenopause (leading up to menopause with decreasing hormone levels), menopause (diagnosed after 12 months without a period), and post-menopause (the time following menopause).
The transition to menopause can be a confusing and difficult time. The changes during this time can heighten vulnerability, as the body undergoes changes, emotional shifts arise, and the concerns about cancer's impact on identity and the future increase.
Am I at risk for gynecologic cancer if I have not gone through menopause?
- Yes. Gynecologic cancers can occur at any age, though the risk increases with age and hormonal changes after menopause.
How do I know if the symptoms I am experiencing are due to menopause or a gynecologic cancer?
- It may be hard to tell the difference but learning about the signs and symptoms of gynecologic cancer, like endometrial cancer or ovarian cancer can help.
- Common symptoms of menopause, like abnormal vaginal bleeding or abnormal bloating, can overlap with gynecologic cancer symptoms.
- Continue seeing your doctor for regular checkups, and bring up any new or worsening symptoms.
Will I go into menopause because of the treatment I am taking or have taken?
- Chemotherapy, surgery (such as a full hysterectomy), radiation and hormone therapy can stop the ovaries from working properly, leading to treatment-induced menopause. This type of menopause can be temporary or permanent.
- The symptoms of treatment-induced menopause are similar to those of natural menopause. These symptoms may include hot flashes, night sweats, fatigue, difficulty sleeping, vaginal dryness, lower sex drive, mood changes, and weight gain.
- If you experience treatment-related menopause, your health care team can help identify supportive treatments that may help you manage any symptoms. Options will depend on your age, cancer type, previous treatment, other health conditions, and your preferences.