You are about to leave OurWayForward.com.
You are about to leave a GSK website. By clicking this link, you will be taken to a website that is independent from GSK. The site you are linking to is not controlled or endorsed by GSK and GSK is not responsible for its content.
Understanding How Family History & Biomarkers Play a Role in Ovarian Cancer
Ovarian Cancer Genetics & Biomarkers
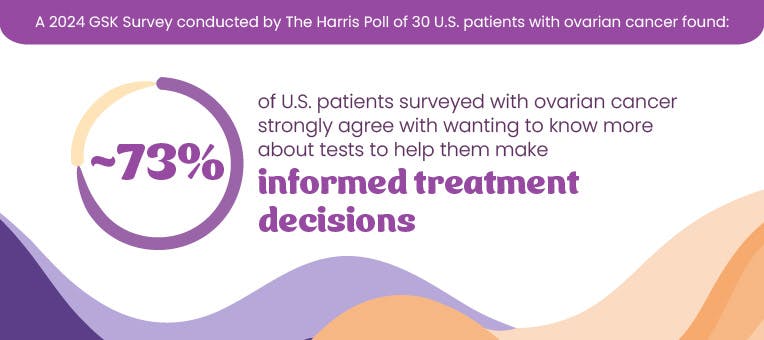
Ovarian cancer can be a genetic disease. This means it can be caused by changes in the genetic components, or genes, which controls how cells grow and divide. Certain genetic biomarkers, or characteristics, can impact the risk of developing certain cancers and inform treatments you may be able to receive. Read on to learn how your family history plays a role, what genetic biomarkers/mutations to look out for, and how to get tested for them.
Family History
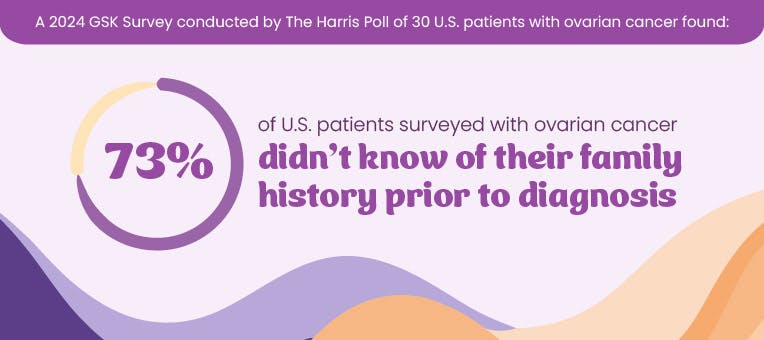
Your genes can determine many characteristics about you, such as the color of your hair, how tall you are, and whether you are at risk of developing certain diseases, such as ovarian cancer. Even though this type of cancer is specific to people assigned female at birth, you can inherit the genes that increase your risk from your mother or your father.
How do I learn more about my family history?
To understand your own health risks, it’s helpful to talk to your family members. Here are some key pieces of information to gather:
- Their sex, date of birth, and ethnicity
- Any medical conditions they know of, and the age they were diagnosed
- Any complications they had during pregnancy or other reproductive issues
- Their lifestyle habits, such as diet, exercise, and tobacco use
It’s also important to understand the health history of any immediate relatives who have passed away.
Other places you can look for information are:
- Public records (birth certificates, death certificates)
- Obituaries
- Baby books
Having these conversations can be challenging. If you’re unsure about discussing health history with your family, consider these tips:
- Don’t go at this alone—ask a sibling or close family member to join you
- Explain why you want to gather this information
- Respect your relatives’ privacy
- Listen without judgment
In addition to talking with family, doctors can perform genetic testing and look for other biomarkers that can sometimes help determine certain cancer risk, prognosis, and treatment.
Ovarian Cancer Biomarkers & Testing
Women with ovarian cancer often have a BRCA gene mutation and/or a tumor biomarker called HRD. There are tests available to help determine your BRCA and HRD status. These tests can help assess your potential risk of developing ovarian cancer or help your healthcare professional determine which treatment option might be best for you.
BRCA is identified through genetic testing, while HRD is determined through genomic testing. Read below to learn some of the basic differences between these tests.
Genetic Testing
A genetic test looks for mutations on specific parts of DNA, called genes, that may have been passed down by a family member
BRCA1 and BRCA2 testing
Testing can be done at any time, before or after diagnosis, though it is typically used to assess potential risk of cancer, particularly if you have a family history
Testing is typically done during a specialized doctor’s office visit and involves taking a blood or saliva sample
Genetic testing can help determine if a person has an increased risk for developing cancer. It does not predict whether someone will develop cancer
VS
Definition
Example
Timing
Method
Significance
Genomic Testing
A genomic test looks more widely at all of your DNA, rather than specific parts of your DNA
HRD testing
Testing is done following cancer diagnosis
Testing is done on the tumor itself and involves taking a sample of your blood or the tumor, via a biopsy or surgery
Genomic testing can help assess personalized treatment down the line
It is important to discuss with a healthcare professional whether these tests are appropriate for you or your loved one, and to discuss any test results with a healthcare professional.
What is BRCA?
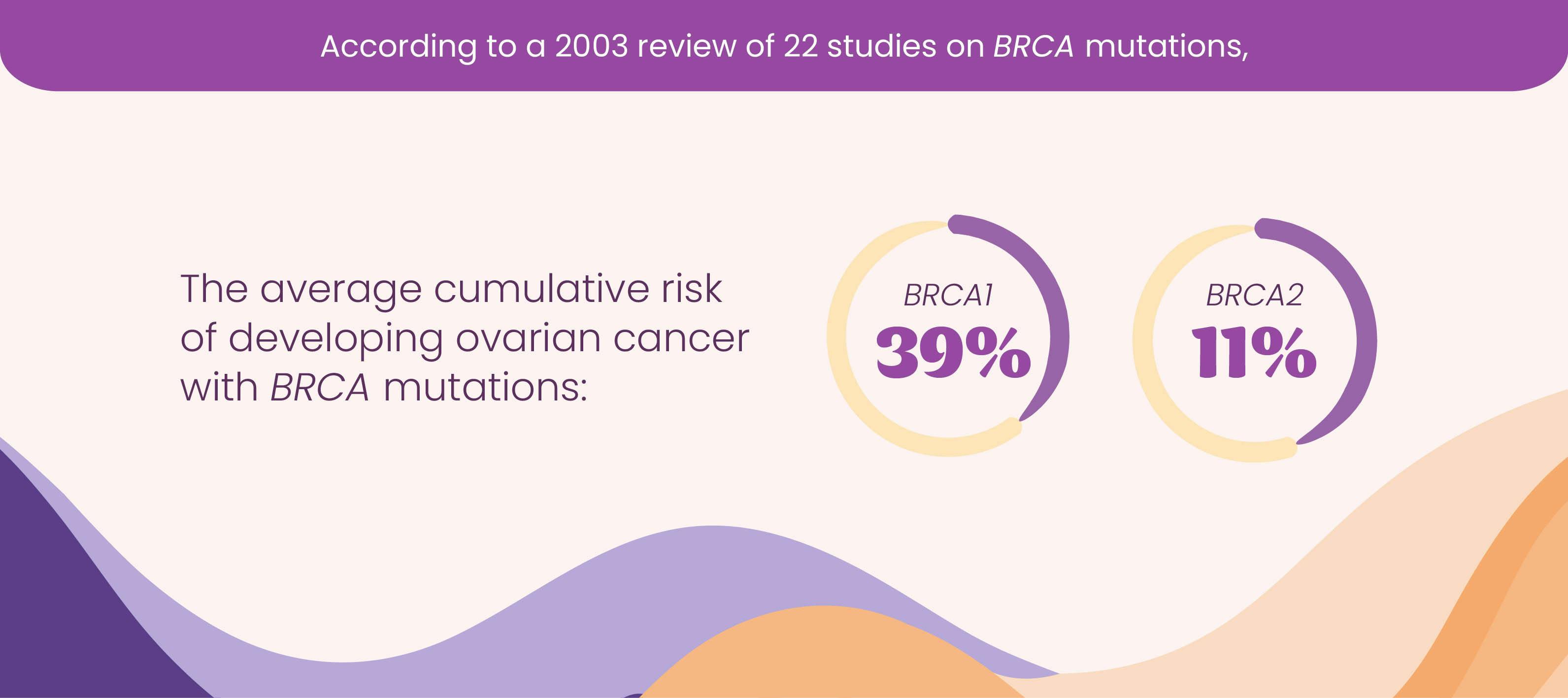
BRCA is an acronym for the BReast CAncer mutation. BRCA1 and BRCA2 are human genes that produce proteins that repair damaged DNA. Every person has two copies of BRCA1 and BRCA2—one inherited from each parent. Normally, BRCA genes protect against cancer, but mutations in these genes can cause them not to work properly, which increases your risk of developing certain types of cancers, such as ovarian cancer. However, nearly 75% of advanced ovarian cancer patients do not have an inherited BRCA mutation.
Who should consider undergoing BRCA1 and BRCA2 testing?
- Those with a family history of breast, ovarian or prostate cancer, especially male breast cancer
- Those with a relative who tested positive for a BRCA mutation
- Those with a previous diagnosis of breast cancer, especially if diagnosed before age 50
- Those of Ashkenazi Jewish ancestry
- Those with a family history of Cowden syndrome, Fanconi anemia, Li-Fraumeni syndrome, Peutz-Jeghers syndrome or other inherited disorders that increase cancer risk
What does having BRCA1 or BRCA2 mean?
If a person has a mutation in either BRCA1 or BRCA2, their chance of getting breast and ovarian cancers during their life goes up. Males with these genetic mutations also have an increased risk of breast and prostate cancers. As soon as you learn about any family history of breast or ovarian cancer, or if you or a loved one were recently diagnosed with breast or ovarian cancer, you are encouraged to talk to your healthcare professional about genetic testing.
How do I undergo BRCA1 and BRCA2 testing?
BRCA testing can be done using a sample of blood or saliva. A member of your healthcare team will take a sample during an office visit and send it to the lab for genetic testing, which looks for mutations in your BRCA1 and BRCA2 genes. Testing for a BRCA gene will not definitively predict whether you will develop cancer, but it can assess your risk.
What happens if I…
Test positive for BRCA1 or BRCA2?
- A positive BRCA test (also referred to as BRCA mutation or BRCAmut) means a person has a mutation in the BRCA1 or BRCA2 gene. A positive BRCA test can indicate whether someone is at a higher risk for developing cancer. This information can also help doctors decide which treatment options may be available for the person.
Test negative for BRCA1 or BRCA2?
- A negative BRCA test (also referred to as BRCA wild type or BRCAwt) means that the gene remains in its original, non-mutated state. It is important to note that even if you are BRCA negative, understanding your status could still play a role in future treatment decisions.
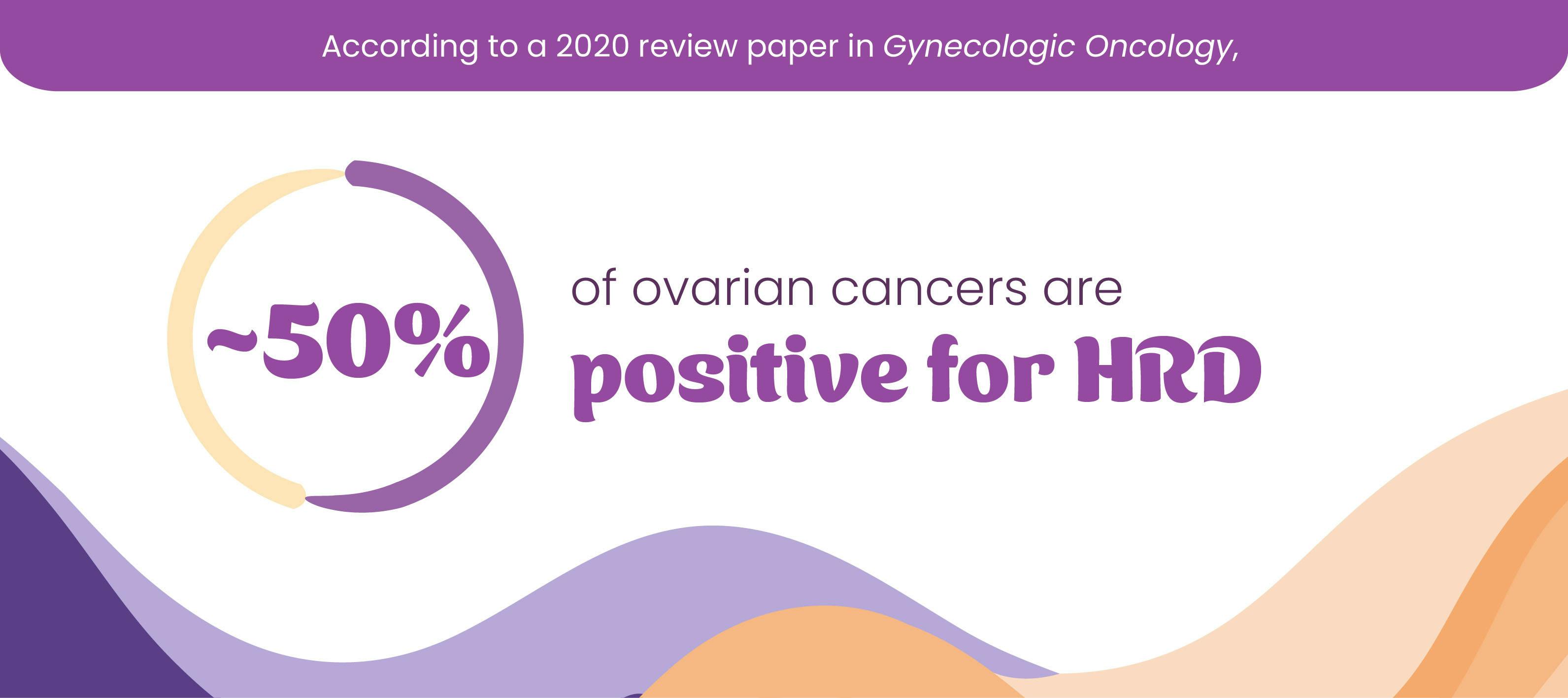
What is HRD?
HRD stands for homologous recombination deficiency. When DNA is repaired under normal circumstances, the process is called homologous recombination. Homologous recombination deficiency happens when this repair system no longer works properly, and therefore is unable to repair damaged DNA. When a cancerous tumor tests positive for HRD, this means that its cancer cells have a harder time repairing themselves, which can make them more vulnerable to treatments that further block this repair mechanism, such as PARP inhibitors.
What does having HRD mean?
HRD is an important biomarker for advanced ovarian cancer, as it can help predict how well the tumor may respond to different treatment options.
How do I undergo HRD testing?
HRD testing in ovarian cancer is done on the tumor itself, either through a biopsy or by testing part of the tumor after it has been removed surgically. The sample is then sent to the lab for genomic testing, which looks at all of your DNA to check for mutations. Genomic testing can help your healthcare team figure out how your ovarian cancer may behave and what treatments might work best against it.
What happens if I…
Test positive for HRD?
- If your tumor is positive for HRD, your healthcare team may consider a variety of appropriate treatment options.
Test negative for HRD?
- Even if you test negative for HRD, there are still treatment options available. Talk to your healthcare professional to learn more about the treatment options you are eligible for.
Is Homologous Recombination Deficiency (HRD) the same as BRCA?
BRCA mutations can cause HRD, but many ovarian tumors that test positive for HRD occur in women who do not have BRCA mutations.
HRD testing is performed on the tumor itself, using a sample of the tumor taken via biopsy or surgery. BRCA testing can usually be done during an office visit and consists of a blood or saliva sample taken by a healthcare professional.
Should I get tested for both HRD and BRCA? When?
You should consult with your healthcare professional about which tests might be most appropriate for you and when. Even if you have ovarian cancer but no family history of it, discussing this testing with your doctor can still be helpful. This testing might help you find out if you qualify for certain treatments.
Biomarker and genetic testing may feel overwhelming, but it can be an essential part of understanding your ovarian cancer risk, prognosis, and treatment options.