You are about to leave OurWayForward.com.
You are about to leave a GSK website. By clicking this link, you will be taken to a website that is independent from GSK. The site you are linking to is not controlled or endorsed by GSK and GSK is not responsible for its content.
What Is Endometrial Cancer?
Endometrial cancer is a type of uterine cancer. It starts in the inner lining of the uterus, known as the endometrium. Uterine cancer and endometrial cancer are often used interchangeably, since endometrial cancer makes up the majority–about 90%–of cancers in the body, or corpus, of the uterus. Endometrial cancer is the most commonly diagnosed type of cancer that affects the gynecologic organs in the United States.
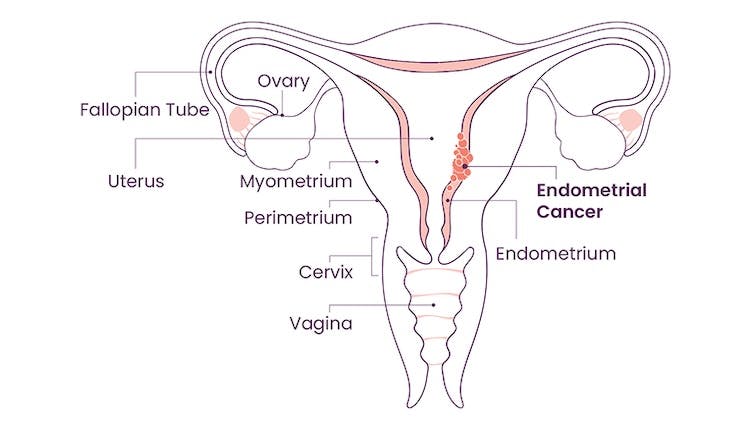
What Does the Endometrium Do?
The endometrium is the lining of the uterus. Throughout each menstrual cycle, the endometrium changes. Typically, once a month, it thickens to prepare for a possible pregnancy. If there is no pregnancy, the lining thins and sheds as a menstrual period. If there is a pregnancy, the lining stays to support it.